All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit Know AML.
The aml Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the aml Hub cannot guarantee the accuracy of translated content. The aml and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The AML Hub is an independent medical education platform, sponsored by Daiichi Sankyo, Johnson & Johnson, Syndax, Thermo Fisher Scientific, Kura Oncology, AbbVie, and has been supported through an educational grant from the Hippocrate Conference Institute, an association of the Servier Group.
Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View AML content recommended for you
QUAZAR AML-001: Update from EHA2021 on survival outcomes according to NPM1 and FLT3 gene mutational status at diagnosis
Featured:
Oral azacitidine (oral-AZA; CC-486) has been approved by both the U.S. Food and Drug Administration (FDA) and the European Commission as a maintenance therapy in adult patients with acute myeloid leukemia (AML). The approvals are for patients who have achieved first complete remission or complete remission with incomplete blood count recovery after intensive chemotherapy and are ineligible for intensive curative therapy, based on the results from the phase III QUAZAR AML-001 trial. The AML Hub has previously reported a series of updates on the QUAZAR AML-001 trial, including the most recent editorial theme on the management of treatment-related toxicities of oral-AZA in patients with AML.
Oral-AZA significantly improved overall survival (OS) vs placebo in the QUAZAR AML-001 trial. However, the subgroup of patients deriving the most benefit from oral-AZA based on prognostic features or mutational profile was not elucidated. NMP1mut is associated with favorable outcomes, particularly in the absence of FLT3-ITD. Subgroup analysis for survival outcomes with oral‑AZA by NPM1/FLT3 mutational status at diagnosis was investigated in the QUAZAR AML-001 trial and the findings were presented by Hartmut Döhner1 during the European Hematology Association (EHA)2021 Virtual Congress.
Study design
The full study design can be found here. Of the total study population (N = 472), 469 patients were eligible for subgroup analysis by mutational status. At AML diagnosis, 137 patients had NPM1mut, 66 patients had FLT3-ITD and/or FLT3-TKD mutations, and 30 patients had co-mutated NPM1 and FLT3‑ITD. Figure 1 shows the NPM1 and FLT3 mutational status at AML diagnosis. The primary endpoints were OS and relapse-free survival (RFS) by mutational status.
Figure 1. Mutational status at AML diagnosis*
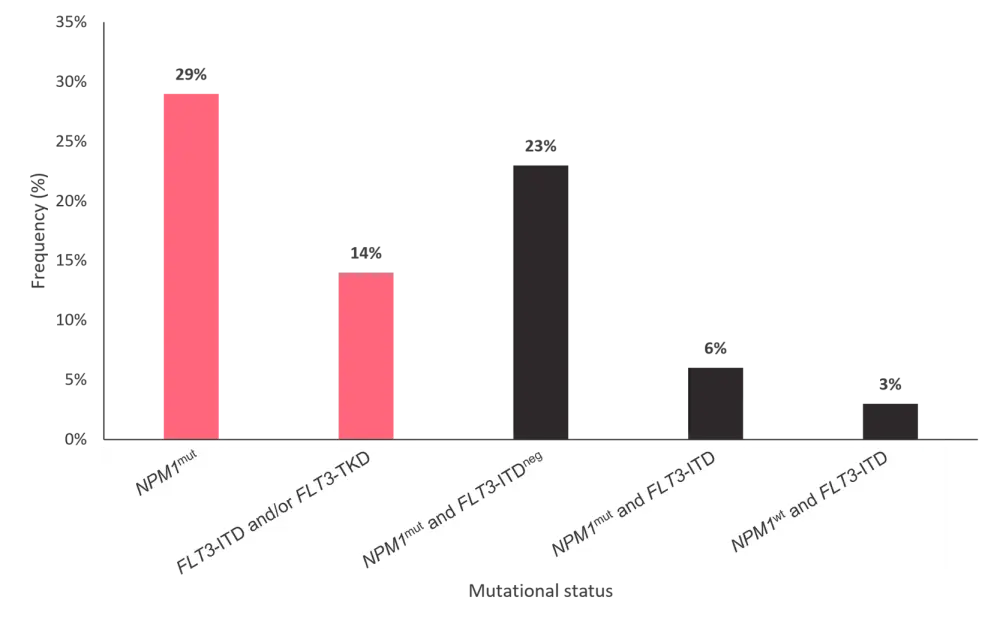
AML, acute myeloid leukemia; ITD, internal tandem duplication; mut, mutant; neg, negative; TKD, tyrosine kinase domain; wt, wild type.
*Adapted from Döhner, et al.1
Results
OS and RFS by NPM1mut status
The median OS was 47.2 months vs 19.6 months (p < 0.001) in the oral-AZA arm and 15.9 months vs 14.6 months (p = 0.032) in the placebo arm for NPM1mut vs NPM1wt, respectively. NPM1mut was predictive of an OS benefit for patients receiving oral-AZA, with a greater increment of improved OS for NMP1mut vs NMP1wt (47.2 months vs 15.9 months) for the oral-AZA arm compared with the placebo arm (19.6 months vs 14.6 months). NMP1 mutational status was similarly prognostic for RFS, with a median of 23.2 months vs 7.8 months (p < 0.001) in the oral-AZA arm and 6.9 months vs 4.6 months (p = 0.011) in the placebo arm for NPM1mut vs NMP1wt, respectively. Patients with NPM1mut at baseline demonstrated more MRD-negativity compared with those with NMP1wt (62% vs 49%, respectively).
OS and RFS by FLT3 status
Although not statistically significant, FLT3 mutational status appeared to confer a negative prognosis in the placebo arm (median OS, 9.7 months for FLT3-ITD/FLT3-TKD vs 15.2 months for FLT3wt; p = 0.351), which was not apparent in the oral-AZA arm (p = 0.715). For patients with FLT3-ITD/FLT3-TKD, median OS (28.2 months vs 9.7 months; p = 0.114) and RFS (23.1 months vs 4.6 months; p = 0.032) were prolonged in the oral-AZA arm compared with the placebo arm, respectively.
OS and RFS by NPM1mut and FLT3-ITD co-mutational status
The negative prognostic impact of FLT3-ITD was observed in the placebo arm (median OS, 11.5 months for NPM1mut + FLT3-ITD vs 18 months for NPM1mut + FLT3-ITDneg) but not in the oral-AZA arm. Patients with NPM1mut + FLT3-ITDneg receiving oral-AZA demonstrated prolonged OS compared with placebo (48.6 months vs 18.0 months). Prolonged OS was also observed in patients receiving oral-AZA with NPM1mut + FLT3-ITD compared with placebo (46.1 months vs 11.5 months)
Multivariate analysis
The prognostic impact of NPM1mut and FLT3-ITD/TKD was independently confirmed with multivariate analysis (Table 1).
Table 1. Multivariate analysis of OS*
|
Comparison |
HR |
p value |
|---|---|---|
|
NPM1mut (n = 137) vs NPM1wt (n = 332) |
0.54 |
<0.001 |
|
FLT3mut (n = 66) vs FLT3wt (n = 403) |
1.54 |
<0.012 |
|
Oral-AZA (n = 236) vs placebo (n = 233) |
0.72 |
0.003 |
|
HR, hazard ratio; ITD, internal tandem duplication; mut, mutation; oral-AZA, oral azacitidine; OS, overall survival; wt, wild type. |
||
Conclusion
This study demonstrated that NPM1 mutational status at AML diagnosis is prognostic and predictive of a survival benefit for patients in remission treated with oral-AZA. On the contrary, FLT3-ITD/TKD mutations had a negative prognostic influence that was only observed in the placebo arm. Oral-AZA improved survival, compared with placebo, for patients in remission with FLT3-ITD/TKD mutations. The influence of NPM1 and FLT3 mutations was confirmed by the multivariate analysis, and oral-AZA showed improvement in OS independent of these mutations.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content


 Sheetal Bhurke
Sheetal Bhurke