All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit Know AML.
The aml Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the aml Hub cannot guarantee the accuracy of translated content. The aml and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The AML Hub is an independent medical education platform, sponsored by Daiichi Sankyo, Johnson & Johnson, Syndax, Thermo Fisher Scientific, Kura Oncology, AbbVie, and has been supported through an educational grant from the Hippocrate Conference Institute, an association of the Servier Group.
Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View AML content recommended for you
Efficacy and safety of decitabine monotherapy vs intensive chemotherapy in older patients with AML
Survival outcomes in older patients with acute myeloid leukemia (AML) have significantly improved with reduced-intensity conditioning followed by allogeneic hematopoietic stem cell transplantation (allo-HSCT). However, it is uncertain whether cytarabine-based standard remission induction chemotherapy (3 + 7) is optimal before allo-HSCT. Lübbert et al.1 recently published the results of a phase III trial of decitabine vs intensive chemotherapy followed by allo-HSCT in older patients with AML (NCT02172872) in Lancet Hematology. Here, we are pleased to summarize the key findings.
Study design and patient population
This open-label randomized controlled trial included 606 patients aged ≥60 years with newly diagnosed AML who were eligible for intensive chemotherapy. The study design and patient characteristics have been previously reported by the AML Hub. The median age was 68 years (range, 60–81 years), and 92% of patients had an Eastern Cooperative Oncology Group performance status of 0 to 1.
- Primary endpoint: Overall survival (OS), defined as time from randomization to death from any cause.
- Secondary endpoints: Rate of complete remission (CR) or complete remission with incomplete hematologic recovery (CRi), progression-free survival, and disease-free survival.
Key findings
- In total, 302 patients received decitabine and 298 received 3 + 7
- Rates of on-protocol allo-HSCT were similar between the decitabine and 3 + 7 groups (40% vs 39%)
- At a median follow-up of 4 years (interquartile range, 2.9–4.8 years), the median OS was 15 months (95% confidence interval [CI], 13–18) and 18 months (95% CI, 14–22) in the decitabine and 3 + 7 group, respectively.
- Figure 1 shows 4-year OS, progression-free survival, and disease-free survival rates.
Figure 1. 4-year survival outcomes*
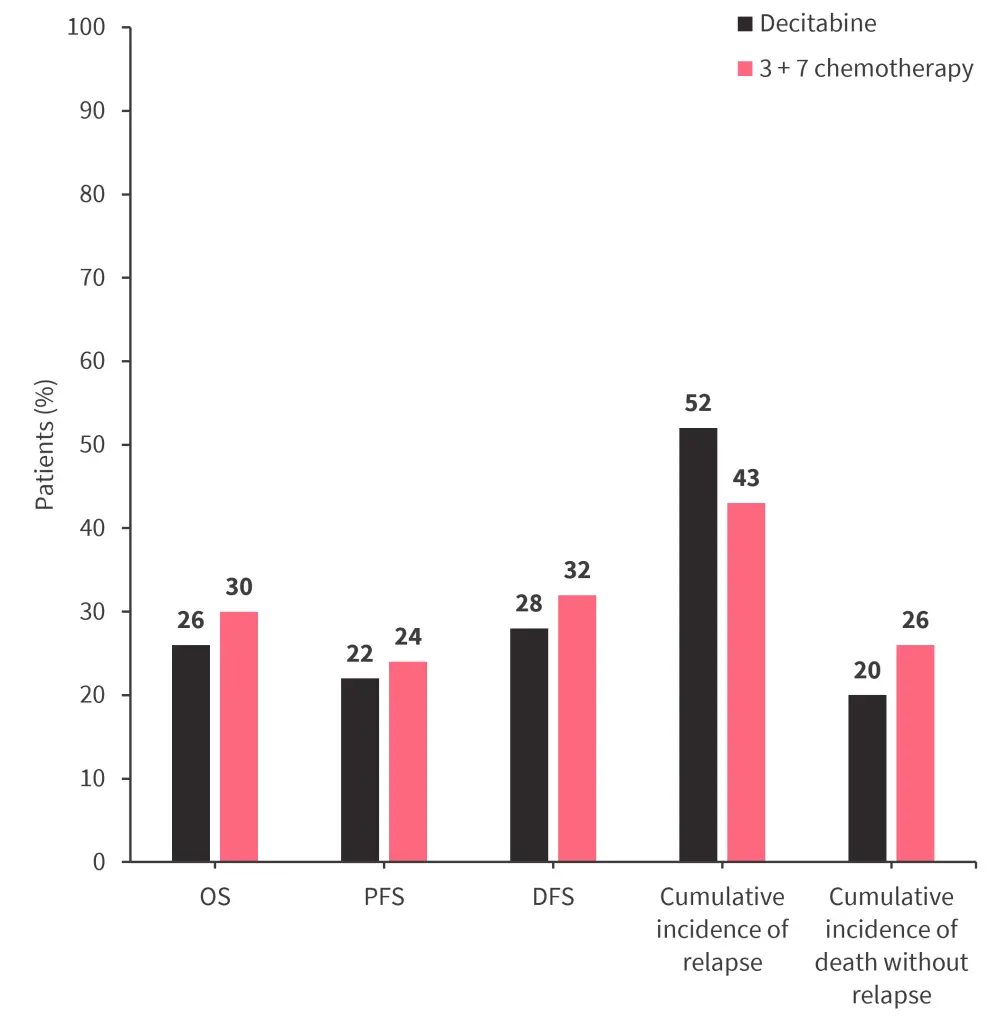
DFS, disease-free survival; OS, overall survival; PFS, progression-free survival.
*Adapted from Lübbert, et al.1
- In the decitabine and 3 + 7 group, CR or CRi was achieved by 48% (95% CI, 42–54) and 61% (95% CI, 56–67) of patients, respectively.
- Following post-protocol treatment, CR or CRi was achieved by 60% and 67% of patients in the decitabine and 3 + 7 groups, respectively (adjusted odds ratio, 0.75; 95% CI, 0.54–1.05).
- Subgroup analysis by age and European LeukemiaNet risk group showed that CR or CRi was higher in the 3 + 7 group compared with the decitabine group, except for patients classified as adverse-risk (Figure 2).
- Patients with mutated NPM1 had a hazard ratio of 2 (95% CI, 0.96–4.17) vs 1.02 (95% CI, 0.77–1.34) in patients with wildtype NPM1 (p = 0.026).
Figure 2. Subgroup analysis: response rates by age and ELN risk group*
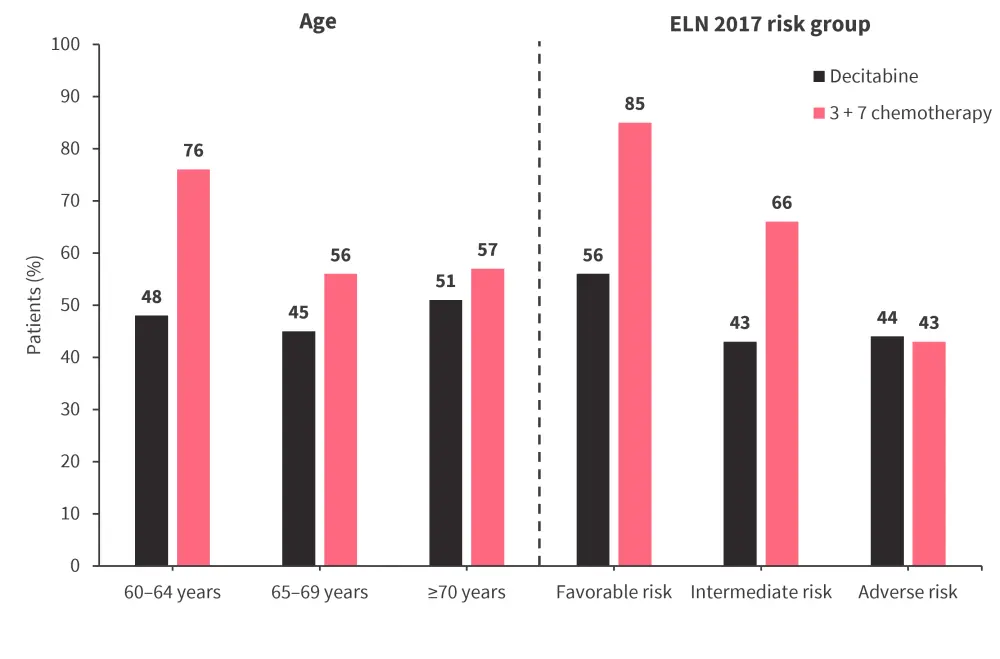
ELN, European LeukemiaNet.
*Adapted from Lübbert, et al.1
- There were 218 deaths in the decitabine group and 205 deaths in the 3 + 7 group (hazard ratio, 1.04; 95% CI, 0.86–1.26; p = 0.68).
- Treatment-related deaths occurred in 12% and 14% of patients in the decitabine and 3 + 7 groups, respectively.
- Grade 3–5 adverse events were lower in the decitabine vs 3 + 7 group (Figure 3).
Figure 3. Adverse events*
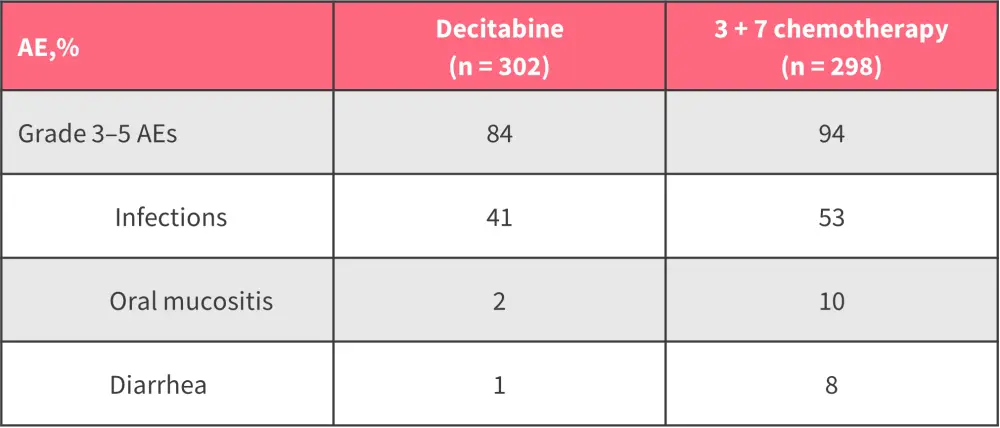
AEs, adverse events.
*Adapted from Lübbert, et al.1
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content


