All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit Know AML.
The aml Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the aml Hub cannot guarantee the accuracy of translated content. The aml and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The AML Hub is an independent medical education platform, sponsored by Daiichi Sankyo, Johnson & Johnson, Syndax, Thermo Fisher Scientific, Kura Oncology, AbbVie, and has been supported through an educational grant from the Hippocrate Conference Institute, an association of the Servier Group.
Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View AML content recommended for you
Gemtuzumab ozogamicin (GO), a CD33-directed antibody-drug conjugate, is approved for the treatment of patients with newly diagnosed (ND) and relapsed/refractory CD33-positive acute myeloid leukemia (AML).1 GO has been shown to improve survival outcomes in patients with AML with non-adverse risk cytogenetics when combined with 7+3 induction chemotherapy, which the AML Hub has previously reported on here and here.2–5 However, more information is required on the benefit of GO in patients with intermediate-risk cytogenetics.1 A higher dose with a fractionated dosing schedule may also improve outcomes and a number of clinical trials are investigating fractionated versus single dose GO treatment in patients with AML.3,4
Several presentations at the 64th American Society of Hematology (ASH) Annual Meeting and Exposition discussed GO in patients with AML. Below, we summarize presentations by Awada,2 Freeman,3 Russell,4 and Döhner,5 on the addition of GO to chemotherapy and fractionated versus single dose schedule in patients with AML.
Retrospective analysis of 7+3 plus GO vs 7+32
Study design and patient characteristics
This study retrospectively analyzed outcomes of 113 patients with ND intermediate-risk AML between those who received 7+3 chemotherapy plus GO (n = 33) and those who received 7+3 therapy only (n = 80) at the Roswell Park Comprehensive Cancer Center, US, between 2015 and 2022. The study endpoints included response, subsequent allogeneic hematopoietic stem cell transplantation (allo-HSCT), relapse after remission, and overall survival (OS). Conventional cytogenetic and fluorescence in situ hybridization analysis was performed and genomic profiling was carried out using next-generation sequencing. Patients received cytarabine and daunorubicin, with or without 3 mg/m2 GO on Days 1, 4, and 7. All patients received prophylactic heparin to prevent hepatic veno-occlusive disease if not thrombocytopenic. Patients in the 7+3 group had a higher frequency of NPM1 mutations (p = 0.01), while the 7+3 plus GO group had more patients with IDH1/2 mutations (p = 0.02) and DNMT3A mutations (p = 0.0001). The median follow-up was 24 months.
Key findings
- Treatment response was higher in the 7+3 plus GO group than in the 7+3 group (Figure 1; p = 0.019).
- Patients who did not achieve complete remission (CR)/CR with incomplete hematologic recovery (CRi) in the 7+3 group had a higher percentage of BCOR/BCORL1 (p = 0.0004) and ASXL1 (p = 0.001) mutations than those who did reach CR/CRi, while patients who reached CR/CRi had a higher percentage of NPM1 mutations (p = 0.007) than patients who did not.
- A similar proportion of patients received subsequent (allo-HSCT) in the two groups (Figure 1).
- Relapse rates after CR/CRi were higher in the 7+3 group than in the 7+3 plus GO group (Figure 1; p = 0.007).
- The median OS was not reached in the 7+3 plus GO group and was 35 months in the 7+3 group.
Figure 1. Response rates, MRD status at the time of CR/CRi, percentage of patients receiving subsequent allo-HSCT, and relapse rates after CR/CRi in the 7+3 plus GO and the 7+3 group*
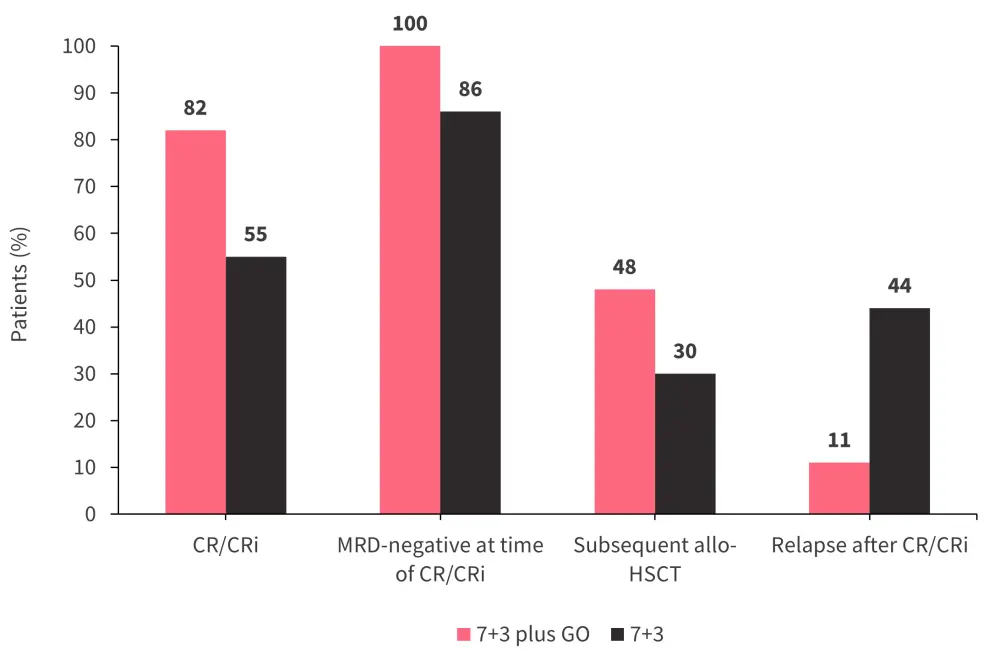
Allo-HSCT; allogeneic hematopoietic stem cell transplantation; CR, complete remission; CRi, CR with incomplete hematological recovery; GO; gemtuzumab ozogamicin; MRD; measurable residual disease.
*Adapted from Awada.2
The addition of GO to 7+3 treatment resulted in higher CR/CRi and lower relapse rates. Whilst the survival benefit was not significant, longer follow-up is justified.
NCRI AML183
Study design and patient characteristics
The NCRI AML18 trial included 844 patients aged ≥60 years with AML or high-risk myelodysplastic syndromes (MDS) without known adverse cytogenetics. Patients were randomized to receive daunorubicin and cytarabine (DA) plus either a single dose of GO (3 mg/m2 on Day 1 of Course 1) or a fractionated dose of GO; (3 mg/m2 [maximum 5 mg] on Days 1 and 4 of Course 1). Following Course 1, measurable residual disease (MRD) was assessed by flow cytometry.
Key findings
- There was no significant difference in 5-year OS rates between the single dose and fractionated dose overall; however, in patients with non-adverse risk cytogenetics, the 5‑year OS rate was higher in patients who received a fractionated dose than in patients who received a single dose (Figure 2; p = 0.045).
- There was no difference in OS advantage from a fractionated dosing schedule by performance status, white blood cell count, or disease type; however, age had a significant impact, with a benefit from fractionated dose in patients aged <65 years and 65–69 years, but with no evidence of an OS benefit of a fractionated dose in patients aged >70 years (p = 0.019).
- 5-year OS rates in patients with IDH1/IDH2 mutations were higher in the fractionated dose group than in the single dose group (Figure 2; p = 0.048).
- In total, 34% of patients who received a single dose of GO and 30% of patients who received a fractionated dose of GO went on to receive allo-HSCT, which conferred an OS advantage (Figure 2; p = 0.007).
- The fractionated dosing schedule group who received allo-HSCT in first remission had longer OS (p = 0.03) and relapse-free survival (p = 0.017) than patients in the single dose group.
Figure 2. 5-year OS rate and allo-HSCT rate in the fractionated versus single dose group*
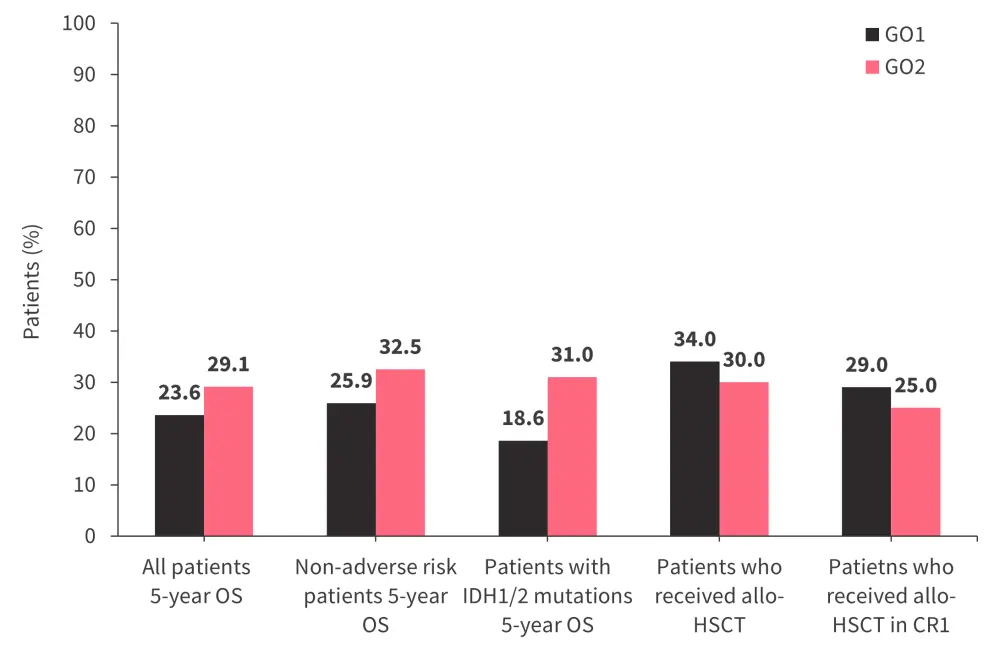
Allo-HSCT, allogeneic hematopoietic stem cell transplantation; CR1, first complete remission; GO1; gemtuzumab ozogamicin single dose; GO2, gemtuzumab ozogamicin fractionated dose; OS, overall survival.
*Data from Freeman.3
- There were no significant differences between the two groups in terms of:
- CR rates (single dose, 57%; fractionated dose, 63%; p = 0.08)
- CR/CRi rates (single dose, 64%; fractionated dose, 67%; p = 0.25)
- Day 30 early deaths (single dose, 8%; fractionated dose, 8%; p = 0.80)
- Day 60 early deaths (single dose, 10%; fractionated dose, 12%; p = 0.38)
- In the 609 patients with available data, lower MRD rates after Course 1 were observed in patients who received a fractionated dose (CR/CRi MRD <0.1%, 64%; CR/CRi MRD negative, 52%; CR MRD <0.1%, 61%; CR MRD negative, 50%) compared with patients who received a single dose (CR/CRi MRD <0.1%, 56%; CR/CRi MRD negative, 47%; CR MRD <0.1%, 50%; CR MRD negative, 42%; p = 0.029).
- The greatest difference in response in favor of fractionated dosing schedule was observed in patients with IDH1 mutations (fractionated dose MRD negative, 63%; single dose MRD negative, 52%) and IDH2 mutations (fractionated dose MRD negative, 59%; single dose MRD negative, 41%).
- Patients who received a fractionated dosing schedule required more units of platelet transfusions (median units, 13) than patients who received a single dose (median units, 11; p = 0.002).
- There was no difference in adverse events between the two groups.
- While platelet recovery was not significantly different between the two groups overall, patients with secondary-like AML mutations who received the fractionated dosing schedule had more days to platelets >100 × 109/L (22 days) than patients who received a single dose (20 days; p = 0.027).
The fractionated dosing schedule of GO was associated with deeper remissions and improved OS in older patients with non-adverse risk genetics when compared with a single dose schedule. There was genetic heterogeneity for differential improvement in leukemia clearance and survival benefit from a fractionated dosing schedule, which was most evident in patients with IDH1/2 mutations. Receiving allo-HSCT in first remission was found to be necessary to translate the improved post-induction response from a fractionated dose schedule into a long-term survival benefit. Most patients aged >70 years did not receive allo-HSCT and there was no evidence of benefit from a fractionated dosing schedule in this group.
NCRI AML194
Study design and patient characteristics
The NCRI AML19 trial included 1,475 patients in the UK, Denmark, and New Zealand with AML or MDS with excess blasts 2 (MDS-EB2) with no known adverse-risk cytogenetics. The patients were randomized to receive either fludarabine, cytarabine, granulocyte-colony stimulating factor, and idarubicin (FLAG-Ida) or DA. Of these, 1,031 patients were randomized to receive either a fractionated dose (maximum 5 mg on Days 1 and 4) or a single dose (3 mg/m2 on Day 1) of GO (Figure 3). Patients with known adverse-risk cytogenetics could enter randomization between FLAG-Ida or liposomal cytarabine-daunorubicin. Post-remission therapy included a second course of FLAG-Ida or DA without GO followed by up to two courses of high dose cytarabine. The median age was 51.5 years. In total, 88% of patients had de novo AML, 7% had secondary AML, and 5% had MDS-EB2. Patients were defined as favorable risk (12%), intermediate risk (75%), and adverse risk (9%).
Figure 3. NCRI AML19 trial schema*
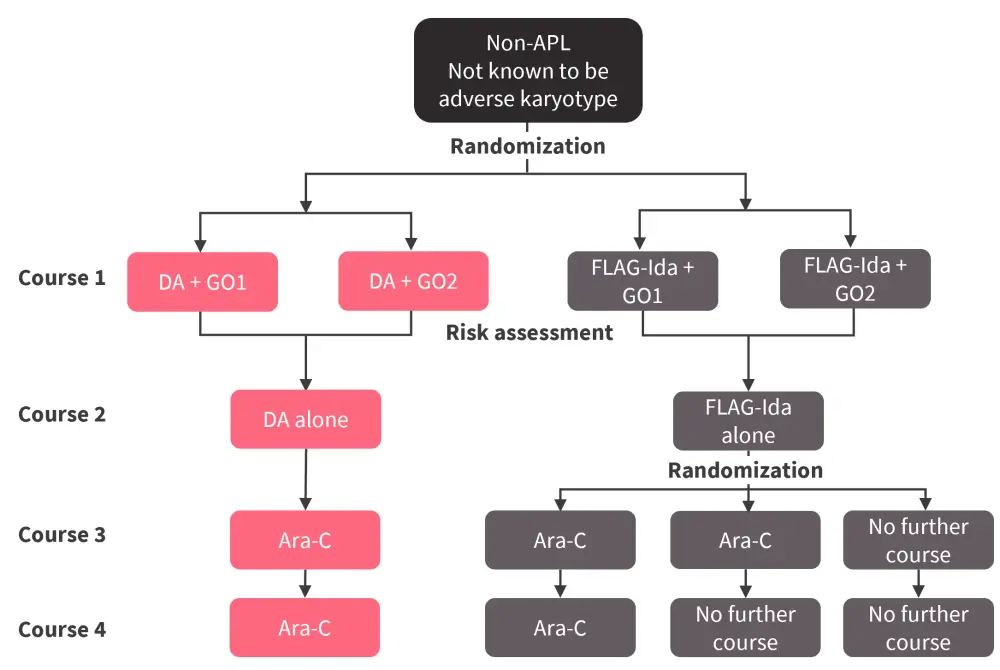
APL, acute promyelocytic leukemai; Ara-C, cytarabine; DA, daunorubicin and cytarabine; FLAG-Ida, fludarabine, cytarabine, granulocyte-colony stimulating factor, and idarubicin; GO1; gemtuzumab ozogamicin single dose; GO2, gemtuzumab ozogamicin fractionated dose.
*Adapted from Russell.4
Key findings
- The CR rate, overall response rate, and 30- and 60-day mortality rates were similar between the FLAG-Ida plus GO and the DA plus GO groups, and between fractionated and single dose GO schedules (Table 1).
Table 1. Response post Cycle 2*
|
CR, complete remission; DA, daunorubicin and cytarabine; FLAG-Ida, fludarabine, cytarabine, granulocyte-colony stimulating factor, and idarubicin; GO, gemtuzumab ozogamicin; GO1, GO single dose; GO2, GO fractionated dose; ORR, overall response rate. |
||||
|
Response, % |
DA-GO |
FLAG-Ida-GO |
GO1 |
GO2 |
|---|---|---|---|---|
|
CR |
86.8 |
87.2 |
— |
— |
|
ORR |
90.7 |
92.5 |
92.3 |
91.2 |
|
30-day mortality |
2.9 |
3.1 |
2.1 |
3.3 |
|
60-day mortality |
4.6 |
4.3 |
3.3 |
5.65 |
- Event-free survival (EFS) and OS rates were similar between fractionated and single dose GO schedules.
- Patients receiving FLAG-Ida had improved EFS compared with patients who received DA (p < 0.001); however, this did not translate into an OS benefit.
- The 5-year cumulative incidences of relapse (CIR) rates were higher in the DA group (44%) than the FLAG-IDA group (25%; p < 0.001).
- The 5-year cumulative incidences of death were higher in the FLAG-Ida group (13%) than in the DA group (7.7%; p = 0.022).
- The 5-year CIR and the 5-year cumulative incidences of death were similar between the single and fractionated dose groups.
- In patients with FLT3 mutations, FLAG-Ida improved EFS and OS (5-year OS, 64%) compared with DA treatment EFS (p = 0.009) and OS (5-year OS, 54%; p = 0.047).
- This survival benefit was greatest in patients with NPM1 co-mutations.
- In patients with NPM1 mutations, FLAG-Ida treatment was associated with improved EFS and OS (5-year OS, 82%) compared with DA EFS (p = 0.003) and OS (5-year OS, 64%; p = 0.005).
- Peripheral blood NPM1 MRD-negativity rates after Cycle 2 were 88% in the FLAG-Ida group and 76% in the DA group.
- Fewer allo-HSCTs were performed in the FLAG-Ida group (46%) compared with the DA group (54%) due to a reduced risk of relapse.
Overall, treatment with FLAG-Ida plus GO improved EFS but not OS when compared with DA plus GO. There was no survival benefit from a fractionated GO dosing schedule compared with single dose. In patients with FLT3 or NPM1 mutations, FLAG-Ida plus GO treatment was associated with improved EFS and OS over DA plus GO.
Expert opinion
What are the updates from the NCRI AML18 and AML19 clinical trials?
During the 4th National Cancer Research Institute (NCRI) AML Academy Meeting, the AML Hub was pleased to speak to Nigel Russell, Guy’s and St Thomas’ NHS Foundation Trust, London, UK. They discuss the latest updates from the NCRI AML18 and AML19 clinical trials.
AMLSG 09-095
Study design and patient characteristics
The AMLSG 09-09 trial included 588 patients aged ≥18 years with ND NMP1 mutated AML. It evaluated intensive induction and consolidation therapy plus all-trans retinoic acid (standard arm) with or without single dose GO; 3 mg/m2 administered in two induction cycles and the first consolidation cycle.
Key findings
Response rates and allo-HSCT rates were similar between the standard arm and the GO arm (Table 2). Furthermore, EFS and OS were similar between treatment arms.
Table 2. Response and allo-HSCT rates post induction therapy*
|
Allo-HSCT, allogeneic hematopoietic stem cell transplantation; CR, complete remission; CRh, CR with partial hematologic recovery; CRi, CR with incomplete hematologic recovery; GO, gemtuzumab ozogamicin |
||
|
Response, % |
Intensive induction and consolidation therapy + all‑trans retinoic acid |
Intensive induction and consolidation therapy + all‑trans retinoic acid + GO |
|---|---|---|
|
CR/CRi |
90.2 |
86.0 |
|
CR |
58.1 |
46.6 |
|
CR/CRh |
72.3 |
66.8 |
|
Refractory disease |
2.4 |
2.4 |
|
30-day mortality |
4.0 |
7.0 |
|
60-day mortality |
6.0 |
9.0 |
|
Allo-HSCT in CR/CRi |
6.4 |
5.5 |
|
Any allo-HSCT during disease course |
37.2 |
28.8 |
Post hoc analysis by age group:
- Post hoc analysis by age group revealed that EFS was higher in the GO group compared with the standard arm in patients aged 18–60 years (p = 0.038); however, this benefit did not translate to OS.
- Patients who received GO had lower rates of CIR than the patients who received intensive induction and consolidation therapy plus all-trans retinoic acid (p < 0.001), which remained true for patients aged 18–60 years (p = 0.002), but not those aged >60 years.
- There was a significantly greater reduction of mutant NPM1 transcript levels after each treatment cycle in patients aged 18–60 years, while there was no consistent effect across treatment cycles in patients aged >60 years.
- Exploratory subgroup analysis revealed a beneficial effect of GO in terms of EFS for female patients, patients aged ≤60 years, patients without FLT3-ITD mutations, and patients with DNMT3A mutations.
The addition of GO to intensive chemotherapy led to lower rates of CIR without an effect on OS, with the beneficial effect on CIR and EFS driven by patients aged 18–60 years. Mutational subgroup analysis showed that patients with NPM1 mutations who were FLT3-ITD wild-type and patients with NPM1/DNMT3A co-mutations significantly benefitted from the addition of GO.
Conclusion
In the retrospective analysis of 7+3 plus GO versus 7+3 in patients with ND intermediate-risk AML, the addition of GO resulted in higher remission rates, lower rates of relapse, and a higher percentage of patients receiving allo-HSCT when compared with 7+3 therapy alone in patients with intermediate risk ND AML.2 Conversely, in the AMLSG 09–09 trial, the addition of GO to intensive chemotherapy did not improve survival outcomes in patients with ND NPM1 mutated AML; although, in patients aged 18–60 years, there were lower relapse rates noted with GO.5
In the NCRI AML18 trial, a fractionated dose schedule of GO was associated with improved survival outcomes compared with single dose in older patients with AML or high-risk MDS with non-adverse risk genetics. However, in the NCRI AML19 fractionated dose GO did not confer a survival benefit over a single dose in patients with ND AML or MDS-EB2.3,4
Age and molecular profile had a significant impact on outcomes across the above studies. Given the variation in study populations, treatments received, and findings, further investigation is warranted to assess the benefit of the addition of GO to chemotherapy and whether a fractionated or single dosing schedule is optimal.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content


 Nigel Russell
Nigel Russell

