All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit Know AML.
The aml Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the aml Hub cannot guarantee the accuracy of translated content. The aml and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The AML Hub is an independent medical education platform, sponsored by Daiichi Sankyo, Johnson & Johnson, Syndax, Thermo Fisher Scientific, Kura Oncology, AbbVie, and has been supported through an educational grant from the Hippocrate Conference Institute, an association of the Servier Group.
Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View AML content recommended for you
The impact of NGS on risk stratification of patients with AML
Genetic analysis is playing an increasingly helpful role in the diagnosis of patients with acute myeloid leukemia (AML) and in the identification of potential targets for therapeutics.1 Cytogenetic karyotype analysis, fluorescence in situ hybridization (FISH), and polymerase chain reaction (PCR) are the standard analysis methods used in the screening of AML-associated mutations. However, with the advent of next-generation sequencing (NGS), new technologies are emerging that may enable more accurate and comprehensive genetic screening. These NGS technologies allow for the sequencing of hundreds of thousands of genes simultaneously in multiple samples and, as we have previously covered on the AML Hub, can be integrated into clinical practice to aid with diagnosis and clinical decision making. However, the accuracy of these new methods, along with their cost- and time-effectiveness, is under discussion.1,2
Below we summarize two recent articles published by Bhai, et al.1 in Molecular Diagnosis & Therapy and by Matos et al.2 in Cancers, which discuss the real-world use of NGS and its impact on risk stratification.
A summary of the study by Bhai, et al.1
This study included a retrospective cohort of Canadian patients with a suspected myeloid malignancy referred for testing between 2018 and 2019.
Results
Patient characteristics
The cohort comprised 1,613 patients, of which 100 were diagnosed with AML (Table 1). The mean age of the total cohort was 63.2 years (range, 3–98.4 years).
Table 1. Patients with myeloid malignancies detected by NGS*
|
AML, acute myeloid leukemia; CML, chronic myeloid leukemia; MDS, myelodysplastic syndromes; MPN, myeloproliferative neoplasms; NGS, next-generation sequencing. |
||||||
|
Myeloid malignancy |
All patients |
Patients >18 years of age |
Patients <18 years of age |
|||
|---|---|---|---|---|---|---|
|
No. of patients |
Patients with gene fusions, % |
No. of patients |
Patients with gene fusions, % |
No. of patients |
Patients with gene fusions, % |
|
|
MPN |
397 |
— |
397 |
— |
— |
— |
|
MDS |
223 |
— |
223 |
— |
— |
— |
|
AML |
100 |
17 |
92 |
16.3 |
8 |
25 |
|
MDS/MPN |
41 |
2.3 |
39 |
2.6 |
2 |
— |
|
CML |
40 |
100 |
38 |
100 |
2 |
100 |
|
Secondary diagnosis† |
812 |
— |
788 |
— |
24 |
— |
Gene fusions
Gene fusions were detected in 58 patients (3.6%), of which 38 were also tested by FISH and 45 by cytogenetic karyotype analysis.
- Among the patients with AML, 17% had gene fusions.
- There was a high degree of concordance between NGS and FISH, with gene fusions in 37 out of the 38 patients detected by NGS confirmed by FISH.
- A KMT2A-MLLT3 fusion in a patient with AML was not detected by FISH.
In the 45 patients karyotyped, 39 patients with NGS-detected gene fusions were confirmed.
Risk classification
Data obtained through NGS were used to stratify patients according to the European LeukemiaNet (ELN) 2017 risk stratification guidelines (Figure 1).
Figure 1. ELN 2017 risk stratification of patients with AML and the mutations detected within each category (n = 100)*
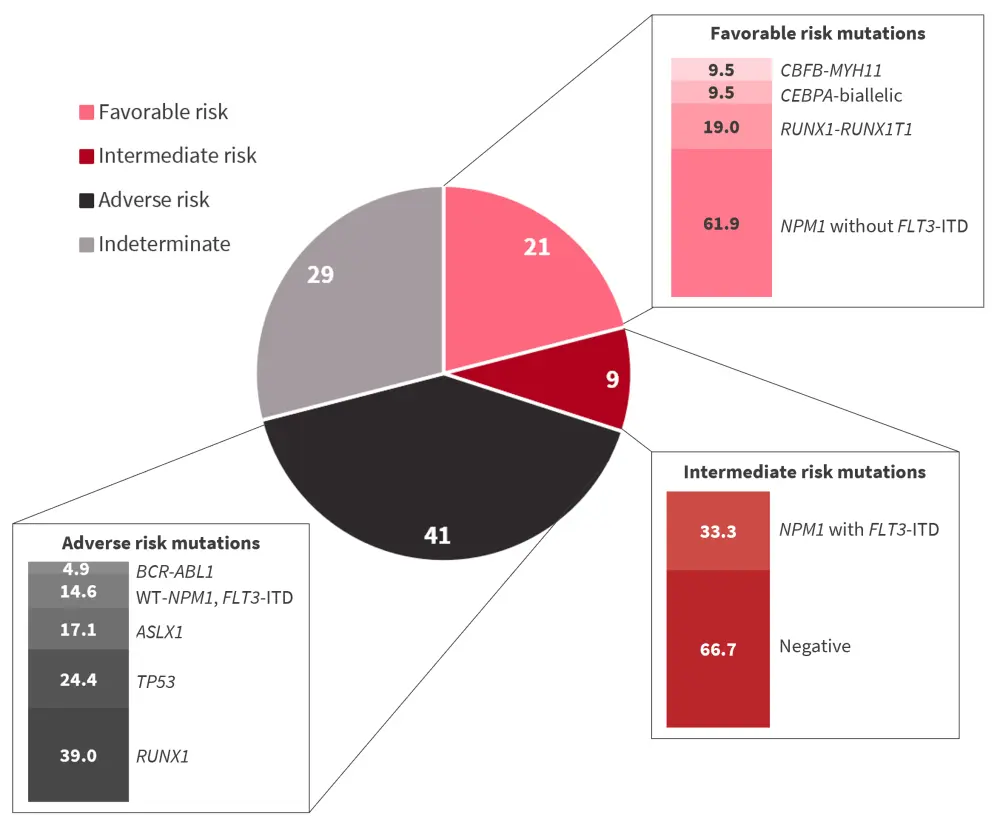
AML, acute myeloid leukemia; ELN, European LeukemiaNet; ITD, internal tandem duplication.
*Data from Bhai, et al.1
When only NGS findings were included, the majority of patients were adverse risk according to the 2017 ELN classification. A large proportion of patients with AML were found to have ≥1 molecular prognostic biomarker (n = 71). Furthermore, NGS showed a high diagnostic yield of 91% in these patients with AML, with a higher rate of prognostic and predictive detection when compared to classic cytogenetic analysis. Classical karyotype analysis classified 37 individuals as having a normal karyotype; however, NGS detected pathogenic variants in 70% of these, of which 27% were in the adverse risk group classification.
Biomarkers
- Patients with IDH and NPM1 mutations frequently had co-mutated DNMT3A; NGS detected these co-mutations simultaneously.
- FLT3 mutations were detected in 12 patients, of which eight were positive for FLT3-internal tandem duplication (ITD).
- The NGS used in this study detected FLT3-ITD at a 2% allele fraction.
- Three patients tested positive for the PML-RARA gene fusion, which was also confirmed by FISH.
A summary of a study by Matos, et al.2
This study prospectively analyzed patients with newly diagnosed AML across five centers in Portugal between 2016 and 2019. Data from NGS were obtained prospectively, with no influence on clinical decisions.
Results
Patient characteristics
This cohort included 268 patients with newly diagnosed AML and one patient with relapsed AML. The median age was 61 years (range, 21–100 years). The gender balance was equal, and 88.5% of patients had an Eastern Cooperative Oncology Group performance status (ECOG-PS) of 0–1, 9.7% had an ECOG-PS of 2, and 1.8% had an ECOG-PS of 3–4. Blood counts were also performed, which revealed a median white blood cell count of 17 × 109/L, median hemoglobin count of 8 g/dL, median platelet count of 47 × 109/L, and median bone marrow blast percentage of 63%.
Risk classification
The study population was classified according to the ELN 2017 criteria before and after the incorporation of NGS data. Without NGS data, 63 patients were unclassified; however, inclusion of these data enabled a further 33 patients to be classified as adverse risk, two as favorable, and one as favorable/intermediate, with 27 patients remaining unclassified. In addition, three patients previously classified as favorable risk, two as favorable/intermediate risk, 20 as intermediate risk, and one as intermediate/adverse risk, were reclassified as adverse risk once NGS data were incorporated (Figures 2 and 3).
Figure 2. Patients in the study population grouped according to ELN 2017 risk classification (N = 269)
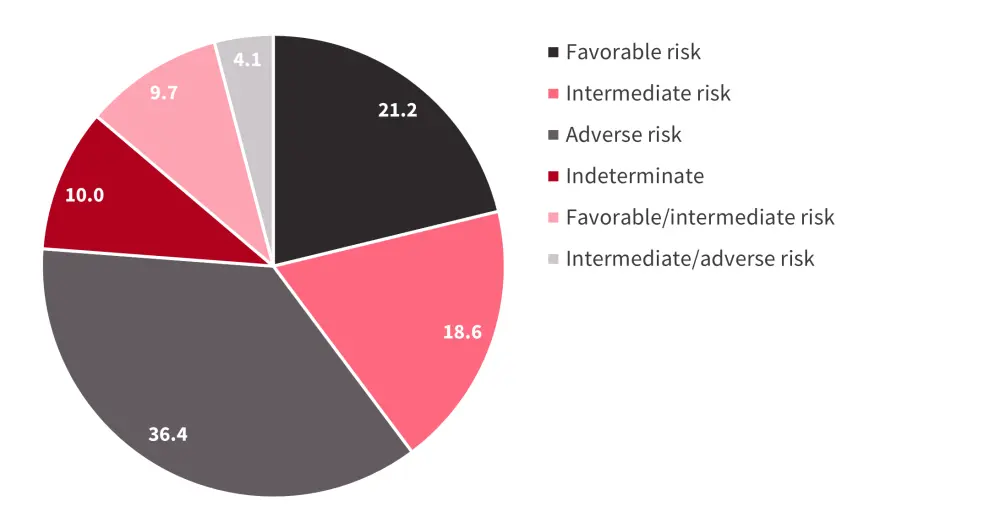
ELN, European LeukemiaNet.
*Data from Matos, et al.2
Figure 3. The mutational landscape of patients in the overall cohort*
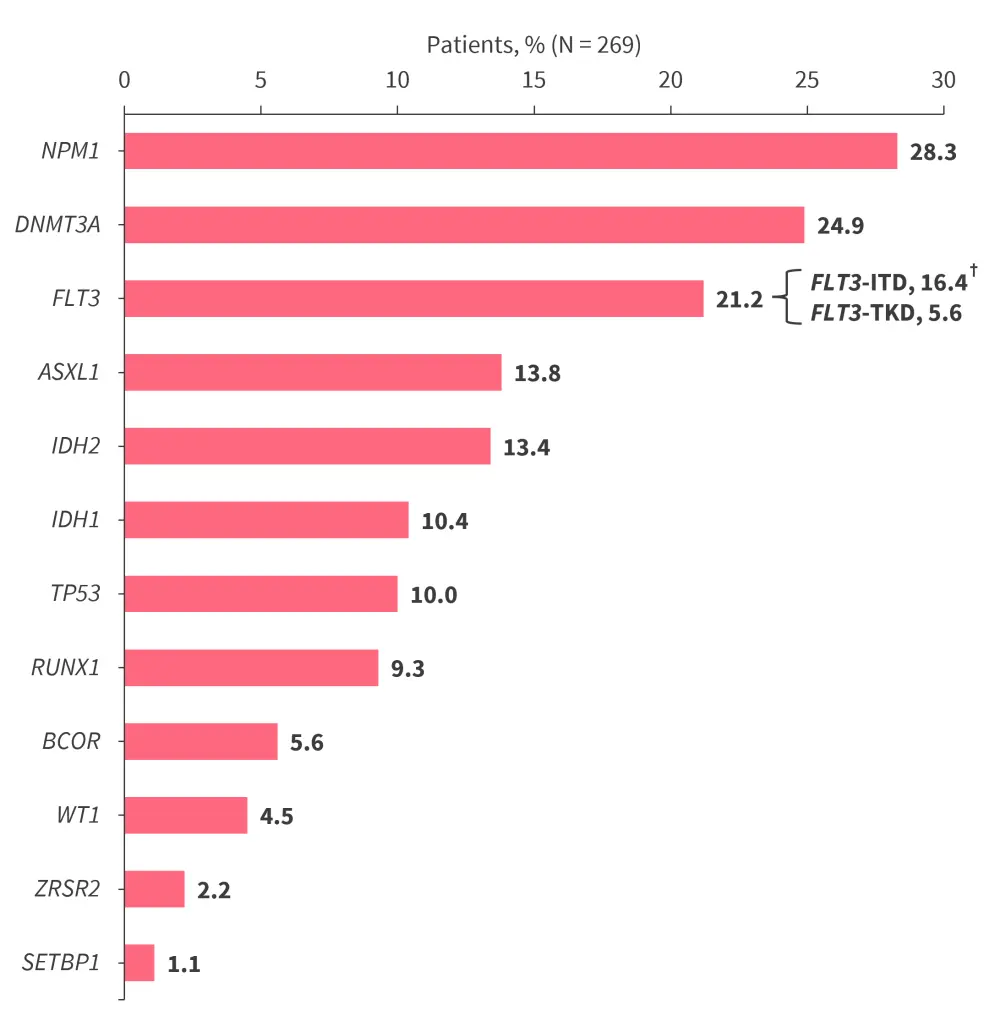
ITD, internal tandem duplication; TKD, tyrosine kinase domain.
*Data from Matos, et al.2
†Two patients had concomitant FLT3-ITD and FLT3-TKD mutations, giving a total percentage of patients with an FLT3 mutation of 21.2%
Biomarkers
When screening for FLT3-ITD mutations, PCR detected 44 positive samples, whereas NGS detected 21. Mutations in the NPM1 gene were identified by PCR in 76 samples and by NGS in 58 samples. However, >50% of FLT3-TKD mutations were only detected by NGS.
- A significant co-mutation rate of NPM1 and FLT3/DNMT3A genes was detected.
- Patients with FLT3 mutations also had high DNMT3A co-mutation rates.
- Patients with BCOR mutations also had high BCORL co-mutation rates.
- TP53 was often co-mutated with complex karyotype alterations.
- NPM1 and TP53, NPM1 and RUNX1, and AXL1 and DNMT3A mutations were mutually exclusive.
Survival analysis
In a multivariable analysis adjusted for age at diagnosis and ELN 2017 risk group, only TP53 mutations were shown to be an independent predictor of adverse overall survival (hazard ratio, 2.96; 95% confidence interval, 1.81–4.84; p < 0.001). Overall survival in the intermediate/adverse group was 30.3 months, unexpectedly longer than the median survival time of the favorable risk group. However, the outcomes for patients with co-mutated FLT3-ITD and DNMT3A in this group were worse, demonstrating the negative impact of co-mutations on prognosis.
Conclusion
Both studies demonstrated the utility of NGS in the diagnosis and classification of real-world patients with AML. Bhai, et al.1 demonstrated a high rate of classification into ELN 2017 risk categories using NGS alone and Matos et al.2 showed that without NGS data ~23% of their study population would be either misclassified or failed risk classification in accordance with the ELN 2017 guidelines. It is important to note that Bhai et al.1 based their risk stratification on NGS alone, whereas Matos et al.2 included both NGS data and alternative molecular tests performed at their centers.
Although NGS has a longer turnaround time (2–3 weeks) than FISH (24–48 hours), it can be used to simultaneously test for multiple relevant biomarkers, which have to be performed separately with FISH.1 When used either alone or in conjunction with classical genetic analysis tools, NGS may provide further insight to aid with the diagnosis and risk stratification of patients with AML and to identify actionable biomarkers.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content


