All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit Know AML.
The aml Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the aml Hub cannot guarantee the accuracy of translated content. The aml and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The AML Hub is an independent medical education platform, sponsored by Daiichi Sankyo, Johnson & Johnson, Syndax, Thermo Fisher Scientific, Kura Oncology, AbbVie, and has been supported through an educational grant from the Hippocrate Conference Institute, an association of the Servier Group.
Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View AML content recommended for you
Optimizing induction therapy in older patients with AML undergoing allo-HSCT
Do you know... Which induction therapy has been shown to provide the most benefit in older patients with newly diagnosed adverse-risk AML undergoing allo-HSCT in first remission?
Survival outcomes in older patients with acute myeloid leukemia (AML) are historically poor, mainly due to factors such as poor tolerance to conventional chemotherapy and a higher incidence of cytogenetic risk in this population.1 Lower-intensity venetoclax-based approaches have shown promising results in older patients with AML who are unfit for intensive chemotherapy (IC). However, the type of induction therapy used in older patients with newly diagnosed AML who are fit for allogeneic hematopoietic stem cell transplantation (allo-HSCT) is controversial and the impact on outcomes remains largely unknown.1
Short et al.1 recently published a retrospective study in Blood Advances evaluating the impact of the type of induction therapy in older patients with newly diagnosed AML after allo-HSCT. We are pleased to present the key highlights from this study here.
Study design
This was a retrospective study in older patients with newly diagnosed AML undergoing allo-HSCT at the University of Texas MD Anderson Cancer Center between November 2012 and July 2021. The study design is shown in Figure 1.
Figure 1. Study design*
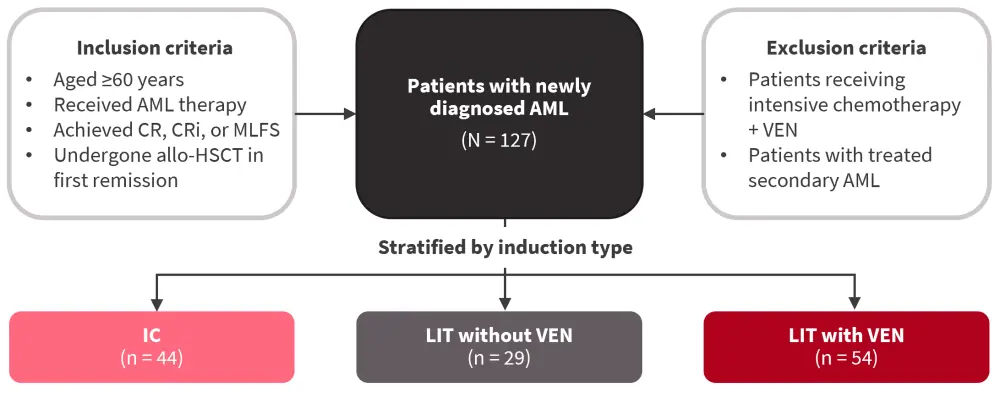
allo-HSCT, allogeneic hematopoietic stem cell transplantation; AML, acute myeloid leukemia; CR, complete remission; CRi, CR with incomplete recovery; IC, intensive chemotherapy; LIT, lower intensity therapy; MLFS, morphologic leukemia-free state; VEN, venetoclax.
*Data from Short, et al.1
Responses, defined by the European LeukemiaNet consensus guidelines were as follows:
- Minimal residual disease (MRD) negativity — absence of a distinct cluster of ≥20 cells showing altered expression of ≥2 antigens
- Relapse-free survival (RFS) — time from allo-HSCT until relapse or death from any cause
- Overall survival (OS) — time from allo-HSCT until death from any cause
- Non-relapse mortality (NRM) — death occurring after allo-HSCT in the absence of relapse
- Graft-versus-host disease — graded per standard criteria
- Cumulative incidence of relapse (CIR)
Results
Baseline characteristics
A total of 127 patients were included, of which 44 patients received IC, 29 received low-intensity therapy (LIT) without venetoclax (VEN), and 54 patients received LIT with VEN. Patients in the IC cohort versus LIT without VEN or LIT with VEN were younger and more likely to have an Eastern Cooperative Oncology Group performance status of 0 at the time of AML diagnosis (p = 0.02) and de novo AML (p = 0.03). Most patients had intermediate or adverse-risk AML; however, two patients had core-binding factor AML in the IC cohort (Table 1).
Table 1. Baseline characteristics*
|
AML, acute myeloid leukemia; ECOG PS, Eastern Cooperative Oncology Group performance status; ELN, European LeukemiaNet; IC, intensive chemotherapy; LIT, lower-intensity therapy; MLFS, morphologic leukemia-free state; VEN, venetoclax. |
||||
|
Characteristic, % (unless otherwise stated) |
IC without VEN |
LIT without VEN |
LIT + VEN |
p value† |
|---|---|---|---|---|
|
Median age (range), years |
63 (60–76) |
67 (61–75) |
68 (60–77) |
<0.0001 |
|
ECOG PS |
|
|
|
|
|
0 |
34 |
10 |
17 |
0.06 |
|
1 |
61 |
72 |
72 |
— |
|
2 |
5 |
17 |
11 |
— |
|
AML type |
|
|
|
|
|
de novo |
80 |
69 |
56 |
0.04 |
|
Secondary |
20 |
31 |
44 |
— |
|
ELN 2017 risk |
||||
|
Favorable‡ |
20 |
14 |
19 |
0.66 |
|
Intermediate |
36 |
38 |
26 |
— |
|
Adverse |
43 |
48 |
56 |
— |
|
Mutations |
|
|
|
|
|
NPM1 |
27 |
24 |
22 |
0.85 |
|
FLT3-ITD |
20 |
24 |
11 |
0.26 |
|
IDH1/IDH2 |
25 |
10 |
26 |
0.22 |
|
KRAS/NRAS |
11 |
10 |
22 |
0.23 |
|
RUNX1 |
7 |
3 |
22 |
0.02 |
|
ASXL1 |
9 |
0 |
17 |
0.06 |
|
TP53 |
18 |
21 |
13 |
0.62 |
Outcomes by induction therapy
The median duration of follow-up post allo-HSCT was 59.8 months, 76.8 months, and 20.3 months in the IC, LIT without VEN, and LIT + VEN cohorts, respectively. The 2-year CIR, NRM, RFS, and OS for all three cohorts are shown in Figure 2.
Figure 2. Outcomes by induction therapy*
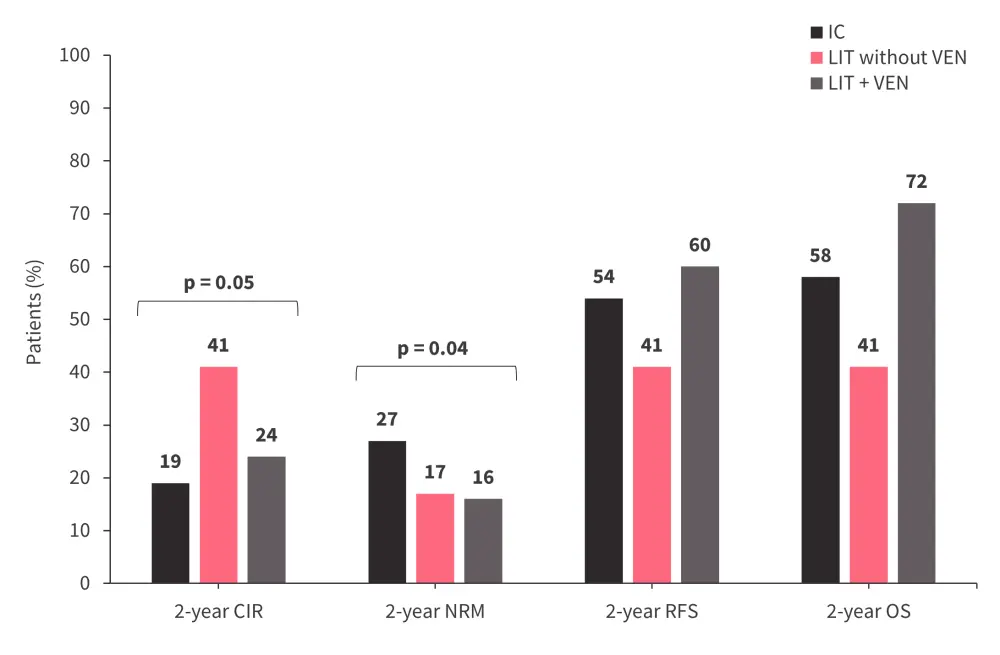
CIR, cumulative incidence of relapse; IC, intensive chemotherapy; LIT, lower-intensity therapy; NRM, non-relapse mortality; OS, overall survival; RFS, relapse-free survival; VEN, venetoclax.
*Data from Short, et al.1
Cumulative incidence of relapse and non-relapse mortality
- Patients achieving MRD negative status prior to allo-HSCT showed a higher CIR in the LIT without VEN versus the IC or LIT + VEN cohorts (45% vs 23% and 17%, respectively).
- In patients with adverse-risk AML, the 2-year CIR was higher in the LIT without VEN versus IC or LIT + VEN cohorts (57% vs 22% and 23%, respectively).
- Patients in the IC cohort showed a higher rate of neutropenic fever compared with the LIT without VEN or LIT + VEN cohorts combined (61% vs 43%, respectively, p = 0.06).
- Patients with TP53 mutations in the LIT without VEN cohort showed a particularly high 1-year CIR of 67% and those in the IC cohort showed a high 1-year NRM of 63%.
Relapse-free survival and overall survival
Figure 3 shows that the 2-year RFS and OS were higher in the LIT + VEN cohort compared with IC and LIT without VEN cohorts in patients with:
- MRD negative status
- Adverse-risk AML
In addition, patients with TP53 mutations in the LIT + VEN cohort also showed improved RFS and OS compared with those in the IC and LIT without VEN cohorts (RFS, p = 0.05; OS, p = 0.02).
Figure 3. Relapse-free survival and overall survival in patients with A MRD negative status and B adverse-risk AML*
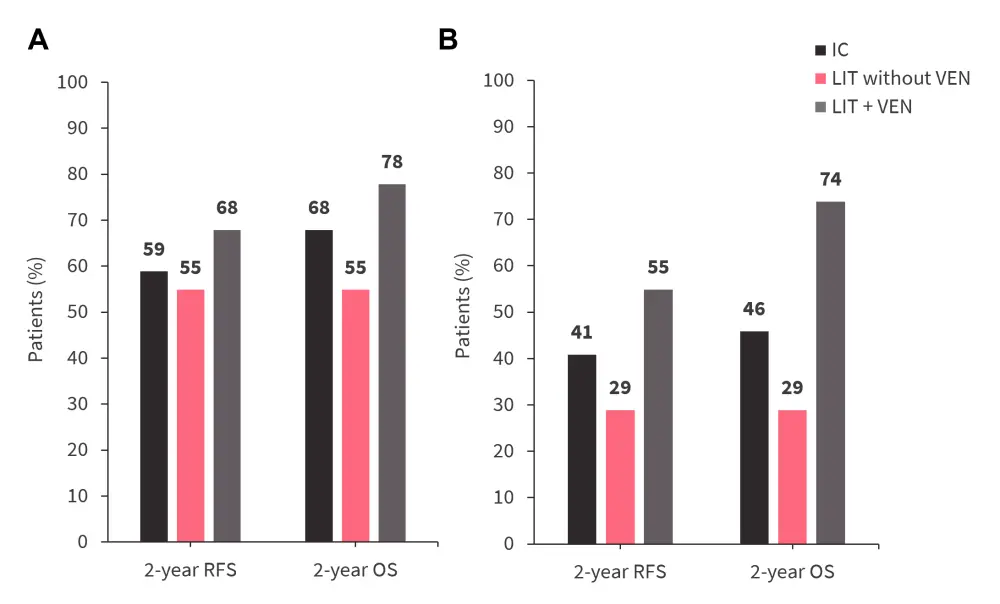
AML, acute myeloid leukemia; IC, intensive chemotherapy; LIT, lower-intensity therapy; MRD, minimal residual disease; OS, overall survival; RFS, relapse-free survival; VEN, venetoclax.
*Adapted from Short, et al.1
In a univariate analysis, HSCT comorbidity index (HSCT-CI) ≥3 was associated with significantly increased risk of relapse (sub-distributional hazard ratio [SHR], 2.21; p = 0.03).
- Patients with adverse-risk AML showed a trend towards increased risk of relapse (SHR, 1.97; p = 0.07) as well as those in the LIT without VEN cohort (SHR, 2.16; p = 0.09).
- Adverse-risk AML (hazard ratio [HR], 1.70; p = 0.05), MRD positivity prior to allo-HSCT (HR, 1.79; p = 0.03), and HSCT-CI ≥3 (HR, 2.54; p = 0.001) were associated with inferior RFS.
- MRD positivity prior to allo-HSCT (HR, 1.78; p = 0.04) and HSCT-CI ≥3 (HR, 2.62; p = 0.001) were associated with inferior OS.
In a multivariate analysis, only HSCT-CI ≥3 was associated with inferior RFS (HR, 1.90; p = 0.02) and OS (HR, 2.09; p = 0.01).
Conclusion
This retrospective study showed favorable RFS and OS with LIT + VEN in older patients with newly diagnosed AML fit for allo-HSCT, providing a rationale to consider LIT + VEN in this population. The study also highlighted better survival outcomes with LIT + VEN compared with IC induction for patients with adverse-risk AML. This appears to be the largest cohort assessing LIT + VEN after allo‑HSCT and comparing IC and LIT + VEN in older allo-HSCT eligible patients. However, the findings of the study should be considered with several caveats such as confounding factors due to younger and fitter patients in the IC cohort and inclusion of patients who underwent allo-HSCT in first remission. The patients in the cohorts were treated in different time periods, and this may have impacted the outcomes due to advances in treatment for relapsed/refractory AML, better supportive care, and changes in allo-HSCT procedures.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

