All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit Know AML.
The aml Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the aml Hub cannot guarantee the accuracy of translated content. The aml and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The AML Hub is an independent medical education platform, sponsored by Daiichi Sankyo, Johnson & Johnson, Syndax, Thermo Fisher Scientific, Kura Oncology, AbbVie, and has been supported through an educational grant from the Hippocrate Conference Institute, an association of the Servier Group.
Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View AML content recommended for you
Efficacy and safety of CLAD and LDAC plus VEN alternating with AZA in older patients with de novo AML
Acute myeloid leukemia (AML) develops mostly in older population and treatment options are restricted due to age and comorbidities in this population. These patients are also poor candidates for intensive induction chemotherapy, therefore, making treatments suboptimal. Early phase trials have shown improved outcomes with low intensity cladribine (CLAD) and low dose cytarabine (LDAC) alternating with a hypomethylating agent (HMA) in this population. The AML Hub has previously reported studies investigating clofarabine or cladribine with LDAC in older patients with de novo AML and venetoclax (VEN) plus HMAs in patients with high-risk AML.
Here, we summarize the key findings from a phase II study investigating the combination of venetoclax with cladribine and LDAC alternating with azacitidine (AZA),1 presented by Patrick Reville from the MD Anderson Cancer Center, Houston, US, during the 63rd American Society of Hematology (ASH) Annual Meeting and Exposition.
Study design1
This was a single center, phase II trial of VEN + CLAD + LDAC alternating with azacitidine in older patients, aged ≥60 years. Eligible patients had de novo AML, were unsuitable for standard induction therapy, had adequate organ function, and an Eastern Cooperative Oncology Group (ECOG) performance status of ≤2. Previous treatment with hydroxyurea, hematopoietic growth factors, tretinoin, or a total dose of cytarabine up to 2 g were allowed.
The treatment cycle comprised of induction and consolidation with VEN + CLAD + LDAC for 4 weeks, and 2 cycles of AZA + VEN for up to 18 cycles (Figure 1). Two cycles of induction with CLAD + LDAC were allowed in patients not achieving CR with first induction cycle. During induction, venetoclax doses were ramped up to 100, 200, and 400 mg for patients receiving strong, moderate, and no CYP34A inhibitor, respectively. All patients received antimicrobial prophylaxis and cytoreductive therapy was given to patients with white blood cell (WBC) count of <20,000 prior to starting venetoclax.
- The primary endpoint was composite complete response (CRc), complete response (CR) + CR with incomplete hematologic recovery (CRi).
- Secondary endpoints included overall survival (OS), disease-free survival (DFS), overall response rate (ORR), and safety profile.
Figure 1. Treatment schema*
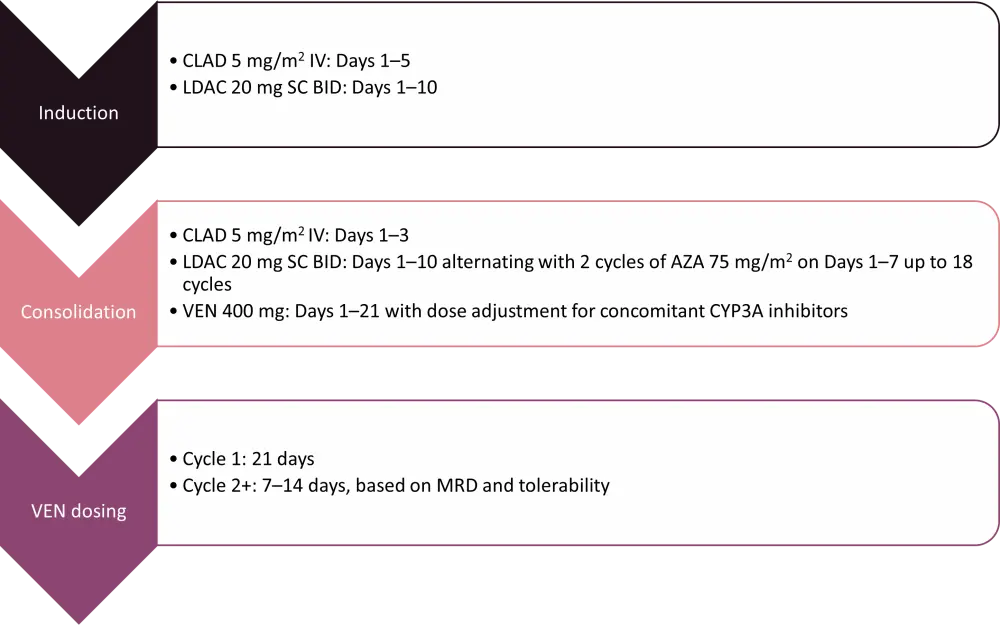
AZA, azacitidine; BID, twice daily; CLAD, cladribine; IV, intravenous; LDAC, low dose cytarabine; MRD, measurable residual disease; SC, subcutaneous; VEN, venetoclax.
*Adapted from Reville et al.1
Results
Baseline characteristics
A total of 60 patients were included, 57% of those were male, and the median age of patients was 68 years (range, 57–84) with 37% patients aged ≥70 years (Table 1).
Table 1. Baseline characteristics*
|
AML, acute myeloid leukemia; ECOG PS, Eastern Cooperative Oncology Group performance status; ELN, European Leukemia Network. |
|
|
Characteristic, % |
Total |
|---|---|
|
ECOG PS |
|
|
0 |
15 |
|
1 |
67 |
|
2 |
18 |
|
Disease type |
|
|
de novo AML |
77 |
|
Secondary AML |
23 |
|
ELN risk |
|
|
Favorable |
23 |
|
Intermediate |
33 |
|
Adverse |
43 |
|
Mutations |
|
|
NPM1 |
33 |
|
DNMT3A |
32 |
|
TET2 |
30 |
|
SRSF2 |
25 |
|
NRAS |
20 |
|
IDH2 |
18 |
|
RUNX1 |
18 |
|
ASXL1 |
15 |
|
TP53 |
7 |
Efficacy
- At a median follow-up of 22.1 months, there was a high CRc rate of 93%, with 80% and 13% of patients achieving CR and CRi, respectively (Table 2).
- The high CR/CRi rates were maintained at 96%, 89%, 75%, 88%, 100% and 93% in patients with ELN adverse risk, adverse karyotype, MLL rearrangements, FLT3 mutated, TP53 mutated, and sAML, respectively.
- 84% of patients had a negative measurable residual disease (MRD) and mortality was low with one and four patients dying at 4- and 8-weeks, respectively.
- Median DFS was not reached, and the estimated 12- and 24-month DFS was 71% and 60%, respectively.
- Similarly, median EFS and OS were not reached, and estimated 12- and 24-month EFS was 68% and 56%, and OS was 73% and 64%, respectively.
- Efficacy of the treatment was sustained in all ELN risk groups with 100% DFS and 93% OS at 24-months in ELN favorable risk group.
- Median DFS was 5.9 months (hazard ratio [HR], 4.56; p = 0.004) and median OS was 15.3 months (HR, 3.97; p = 0.016) in patients with positive MRD vs patients with negative MRD.
- Median DFS was 18 months (HR, 1.63; p = 0.27) and median OS was not reached (HR, 1.50; p = 0.35) in patients aged ≥70 years vs <70 years.
- Patients receiving allogeneic hematopoietic stem cell transplantation (allo-HSCT) showed improved DFS (HR, 0.31; 95% CI, 0.09–1.07; p = 0.064) and OS (HR, 0.28; 95% CI, 0.06–1.24; p = 0.093)
Table 2. Best responses*
|
Allo-HSCT, allogeneic hematopoietic stem cell transplantation; CR, complete response; CRc, composite complete response; CRi, complete response with incomplete hematologic recovery; MRD, measurable residual disease; NR, no response; ORR, overall response rate; PR, partial response; IQR, interquartile range. |
|
|
Response, % |
Total |
|---|---|
|
Best response |
|
|
CR |
80 |
|
CRi |
13 |
|
NR |
5 |
|
Died |
1.7 |
|
ORR (CR + CRi + PR) |
93 |
|
CRc rate (CR + CRi) |
93 |
|
Patients requiring re-induction cycle (n = 57) |
7 |
|
MRD at response assessment (n = 51) |
|
|
Negative |
84 |
|
Positive |
16 |
|
Median number of treatment cycles (IQR) |
3.0 (2.0–5.0) |
|
Responders receiving allo-HSCT (n = 56) |
34 |
|
Mortality rate at 4 weeks |
1.7 |
|
Mortality rate at 8 weeks |
6.7 |
Safety
- The most frequent Grade 3 or 4 nonhematologic adverse events (AEs) was febrile neutropenia (55%), pneumonia (23%), and allergic reaction (3%).
- Grade 4 tumor lysis occurred only in one patient.
- Median time to absolute neutrophil count (ANC) recovery of >500 and >1,000 was 25 and 27 days, respectively, and median time to platelet recovery of >50,000 and >100,000 was 21 and 24 days, respectively.
Conclusion
This phase II study demonstrated that the combination of cladribine with LDAC plus venetoclax alternating with azacitidine was well tolerated among older patients with de novo AML and was an effective treatment option. High rates of responses were observed with durable MRD negativity along with encouraging rates of OS and DFS. The efficacy attained using cladribine with LDAC plus venetoclax alternating with azacitidine was comparable to the outcomes in patients <70 years with AML. However, further studies are warranted to investigate this combination in younger patients not eligible for intensive chemotherapy, as well as comparison with standard frontline therapies.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

